General Information
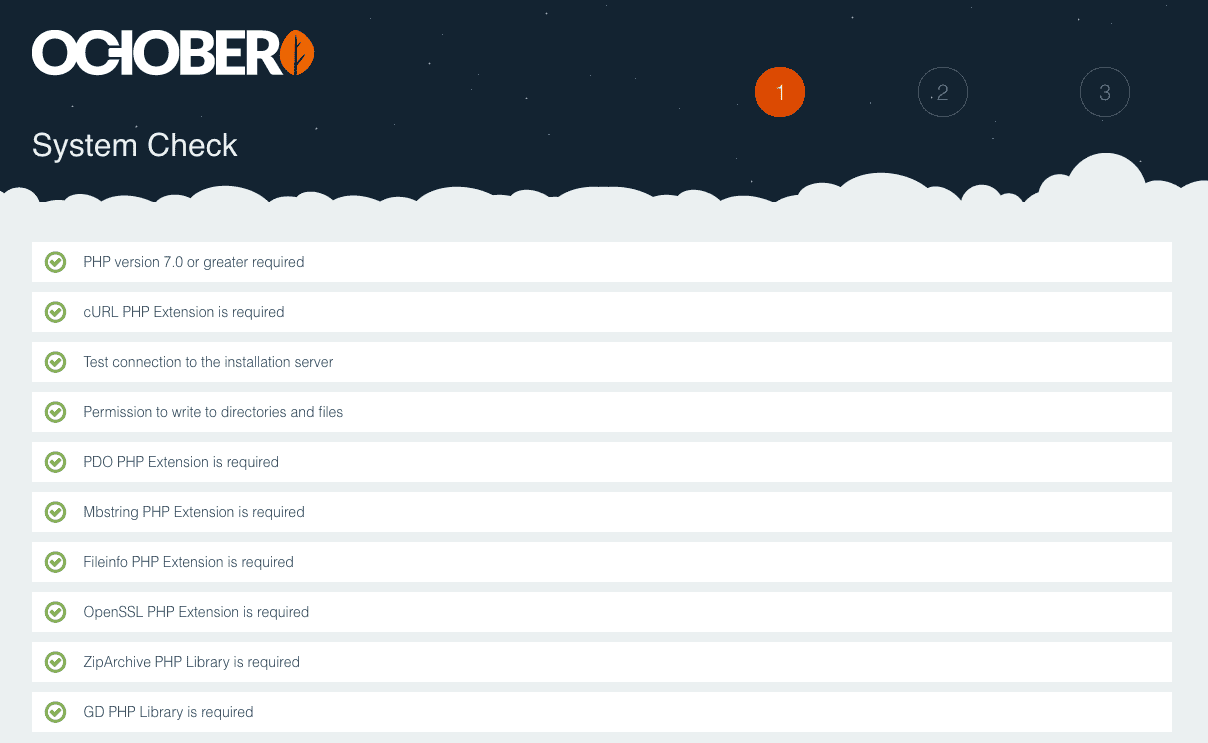
Mac Cms Getshell
The purpose of the Medicaid Administrative Claiming (MAC) program is to provide State affiliated public agencies such as Local Health Districts (LHD's) in Texas the opportunity to submit reimbursement claims for administrative activities that support the Medicaid program. In order for the cost to be allowable and reimbursable under Medicaid, the activities must be found to be necessary for the proper and efficient administration under the Texas Medicaid State Plan, and must adhere to applicable requirements as defined in State and Federal Law.
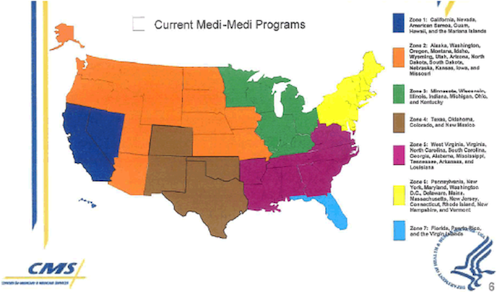
Mac users interested in Cms dvr client software mac osx generally download: UMS Client (v1.0.9) 1.0 Free UMS Client lets you remotely monitor and control your video security system directly from your Mac. Medicaid and CHIP (MAC) Learning Collaboratives The Centers for Medicare and Medicaid Services (CMS) established the Medicaid and CHIP Learning Collaboratives (MAC Learning Collaboratives) to achieve high-performing state health coverage programs, a goal that requires a robust working relationship among federal and state partners.
- Cms free download - webEdition CMS, HP DesignJet 1050C and 1055CM Drivers, MoveCM, and many more programs. Get this HP Design Jet 1050C and 1055CM printer drivers for Mac.
- Welcome to the web site for the Ohio Medicaid Fee-For-Service (FFS) MAC program. This site is dedicated to providing the most current MAC lists for Medicaid drug reimbursement. All past MAC updates are listed here chronologically. In addition, you will find helpful references to material from CMS and the Ohio Department of Medicaid.
LHD's can be reimbursed for certain medical and health-related activities such as outreach services delivered to clients within the community, regardless of whether the client is Medicaid eligible or not, and without any impact on other similar services the patient may receive elsewhere. Outreach services may be provided to a client and/or the client's family and may include activities such as coordinating, referring, or assisting the client/family in accessing needed medical/health or mental care services.
Revenue generated from MAC claims is dedicated to the provision of health services and may be used to enhance, improve and/or expand the level and quality of health/medical services provided to clients within the community. All MAC (Medicaid Administrative Claiming) expenditures which are subject to reimbursement are Title XIX funds. The MAC reimbursements payments received from Medicaid Administrative Claims CFDA #93.778 are subject to the Single Audit Act. Therefore, the funds should be included on the SEFA (Statement of Expenditures of Federal Awards) on each entity's audited financial statements. If the MAC award is identified as a major federal program, the entity's external auditor should perform work deemed necessary to reduce risk and report the funds appropriately in accordance with OMB Circular A-133. The auditor should research all other requirements to ensure that MAC funds are appropriately audited and reported.
Additional Information
What is Medicaid Administrative Claiming for LHD's? (.pdf) (updated 08/17/2020)
Cms Mac For Alabama
Related Information
Guides / Manuals / Tutorials
MAC Financial Participation Guide (.pdf) - effective October 1, 2010
MAC Financial Guide (.pdf) - effective through September 30, 2010
MAC Video Tutorial - effective October 15, 2015
Mac Cms Software
Time Study and MAC Guide (.pdf)
Medicare Macs By State
Notices
Cms Mac For Pennsylvania
View a list of important notices regarding Medicaid Administrative Claiming for Local Health Districts.
Cms Mac For Texas
Participation Documents
Contracting Information
The purpose of the Medicaid Administrative Claiming (MAC) program is to provide State affiliated public agencies in Texas the opportunity to submit reimbursement claims for administrative activities that support the Medicaid program. In order to participate in the MAC program, the LHD provider must be a public entity and enter into a MAC contract with the Texas Health & Human Services Commission (HHSC).
In addition to the contracting process, each LHD provider must also have an active Texas Provider Identifier (TPI) and/or National Provider Identifier (NPI), meet HHSC training requirements and participate in the Random Moment Time Study (RMTS), which includes the certification of the participant list and participation in the time study. To enroll as a Medicaid provider, please complete the Texas Medicaid fee-for-service provider enrollment form on the Texas Medicaid and Healthcare Partnership (TMHP) website:
An LHD provider that is interested in participating for this upcoming Federal Fiscal Year (FFY) should consider beginning the process as soon as possible, as it may take many months to complete all paperwork and training requirements.
Listing and links to all forms required for participation in the MAC program by LHD's.
Training
The link below contains information regarding the LHD training information. It is IMPORTANT to carefully read all the information provided so as to fully understand who must attend 'initial' training and who is eligible to take 'refresher' training.